Abstract
Background
Risk of recurrence of Solitary plasmacytoma (SP) or progression to Myeloma (MM)/ multiple plasmacytomas (MP) is well established. Standard risk factors (RF) for disease recurrence/ progression include: patient age, SP size, axial location, bone marrow (BM) plasma cell %, and abnormal serum free light chain (SFLC) ratio at diagnosis and M protein persistence post radiotherapy (RT). Data is limited on whether functional imaging parameters can serve as a biomarker for risk of recurrence/progression.
Methods:
We conducted a retrospective analysis of 66 SP patients (23 UK, 43 Brazil) over a 15 yr period. We recorded patient and disease characteristics at baseline including SFLC, BM examination, imaging by skeletal survey, CT/MRI and functional imaging by 18F-FDG PET CT or 99mTc-Sestamibi MIBI(SPECT/CT or planar). Follow-up (FU) functional imaging was performed as routine surveillance or suspicion of disease recurrence/progression. The proportion of patients progressing to MP/ MM was recorded. Disease recurrence/progression was defined as the detection of new SP/ MP on FU functional imaging or biochemical relapse. Effect of surgery and RT on disease recurrence/progression was analysed. PFS and OS from diagnosis and time of repeat functional imaging were measured using Kaplan-Meier estimates. Factors examined for their predictive value of progression risk included: initial SP size, location, surgical resection, RT dose, baseline SFLC, functional imaging findings and clinical context of repeat scanning. Log-rank test was used for univariate testing and multivariate Cox analysis.
Results
Median patient age was 60 yrs (19-82 years). SP location was bone (83%) and extramedullary (EMP) (19.7%). Median SP size was 60mm (range 19-220mm). BM results were available for 56/66 patients, median PC % 0.1% (range 0-9.2%, IQR 0-2.9%).
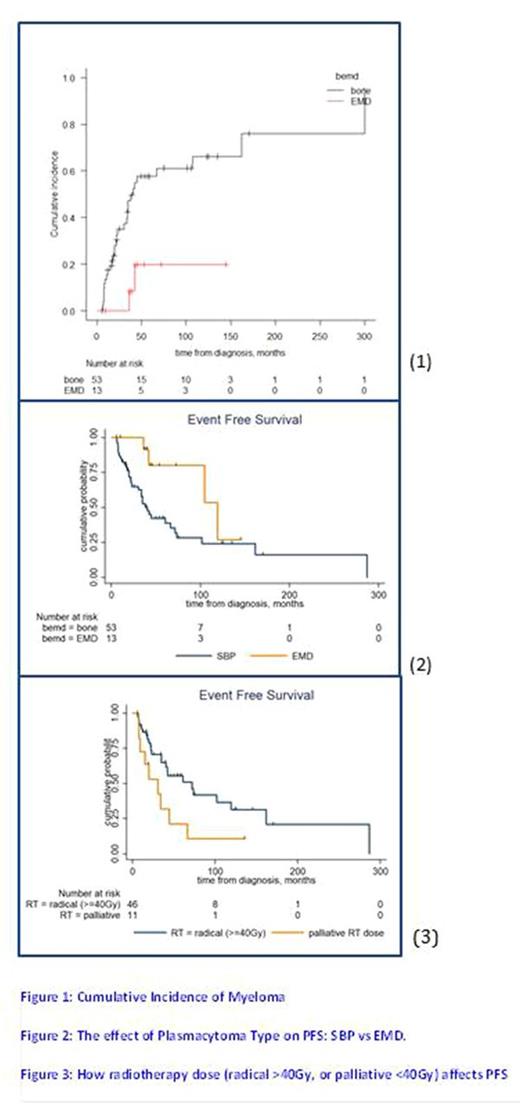
Median FU 53.6M (range 5.8-327 months) with 9 deaths (6/9 disease progression related). On FU 31/66 patients (47.0%) never progressed. One patient (7.7%) had recurrent SP in EM location, 6 (11.3%) as bony SP and 28 (42.4%) progressed to MM/MP. The cumulative incidence of progression to MP/ MM was 49.9% at 5 years (95% CI 35.6-62.6%), bone SP 57.7% (95% CI 21.7-48.6%) EMP 19.8% (95% CI 2.4-49.4%) (fig. 1).
OS was 90.7% (95%CI 79-96%) 5 yrs from diagnosis, median PFS was 61M with no significant difference in PFS or OS between centres. RFs for progression to MM included bone SP compared to EMP (log rank p=0.0265)(fig. 2). Size of SP had no effect on outcome. Baseline SFLC correlated positively with lesion size but was not predictive of outcome.
57/66 (86.4%) received RT, either radical (≥40Gy N=46, 80.7%) or "palliative" dose (<40Gy, N=11, 19.3%). Patients treated with less than 40 Gy showed more PFS events, (chi-square 4.61, p=0.032)(fig. 3). Surgical resection had no effect on PFS (p=0.5). 6 patients received systemic chemotherapy at presentation, 5/6 remain in remission after a median follow-up of 10yrs.
All patients in the UK cohort had PET-CT (n=23), the Brazilian cohort was imaged by MIBI (n=11). FU imaging was performed in 62.1% cases at a median of 174 days ~ 6 months post diagnosis. 16 patients (39%) were scanned on suspicion of relapse, 9/16 (56.2%) showed progressive disease. 20 patients (48.7%) were scanned as routine surveillance, one patient (5%) showed disease progression. FU PET SUVmax was not useful in predicting outcome.
The positive predictive value of FU imaging to determine clinical outcome was high (100%) regardless of if the scan was for surveillance/suspected progression. Negative predictive value was low (60%, 95%CI: 40.6%-77.3%) and particularly poor (14.3%, 95%CI: 0.4-58%) in suspected relapse, suggesting more diffuse infiltration in BM.
Conclusion
This large retrospective dataset of SP patients from UK and Brazil shows no difference in PFS and OS despite variability in racial distribution and access to treatment. We have confirmed bony location and use of <40GY as RFs for disease progression. SFLC ratio and size of SP were not RFs for progression. Based on our results use of upfront adjuvant chemotherapy is worth prospective evaluation (IDRIS trial in UK). Our data suggests functional imaging should be used when there is suspicion of relapse/progression and not as a routine surveillance tool. Observations from our large real world plasmacytoma cohort regarding value of functional imaging are hypothesis generating, but need confirmation prospectively.
Ramasamy: Celgene: Honoraria, Other: Research Grant; Janssen: Honoraria, Other: Research Grant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal